 Are you overwhelmed with the operations-side of running a practice? Have you inherited a mixed bag of useful practice tips coupled with antiquated and even incorrect guidance?
Are you overwhelmed with the operations-side of running a practice? Have you inherited a mixed bag of useful practice tips coupled with antiquated and even incorrect guidance?
Would you benefit from a how-to manual from start-to-finish, coaching you along the way in the development of your practice? Can you use a resource that bridges to the higher level you aspire to?
Building on my 28 years of experience in practice, coupled with speaking to hundreds of practitioners across North America, I’m putting together a progressive Practice Operations workbook for massage therapists.

Each module provides theoretical constructs, real-life examples and reflective exercises to move you forward while honouring your past.
The best resource, of course, would be designed by you…for you. Even if you’ve been in practice for many years (and perhaps especially for you), I want to reconfigure your feelings of isolation and frustration. If you’re closer to the entry-level part of practice, all the better. You can start off on the right foot and fast-track your progression.

Here’s what I need from you: Have a look at this rough outline. Would this progressively meet your needs, at whatever stage you’re at? What specifically would you like to see included in the program?
What have been your practice challenges? What pearls of wisdom would you like to share with others?
Entry-Level: Practitioner Physical and Security Needs
1) Profile – We start with you. Reflective exercises tease out personal and professional talents that demonstrate your unique competence, experiences and skillsets as you lay the foundation upon which to build your professional career.
2) Provisions – Account for all assets you bring to the table – capital, contacts, business competence as commitment to see it through. Evaluate if you have sufficient resources to launch your own practice, or would instead excel apprenticing in an established enterprise.
3) Purpose, Passion, Position in the Marketplace and Workplace – What do you bring to the marketplace? Why does your product/service matter? What populations do you serve? What is your role in the workplace? What are the values that guide your practice? We drill down to your core beliefs so you can best position your practice launch.
4) Product, Pricing and Place – Define your “product” and how it will be packaged and presented. Consider pricing theory and strategies while you contemplate the place (sector/delivery-of-care model) you will incorporate in your practice.
5) Promotion – Learn how to recruit prospective patrons, retain them for the long-term, reward patron behaviour that builds your practice, and re-serve (serve again) those patrons who would buy more from you.
6) Profit – Track key financial metrics, build financial competence, nurture growth and positive cash flow. Unless your practice is just a hobby, you’ll need profit for growth, contingency and retirement.
Established: Professional Esteem, Relationships and Processes
7) and 8) Practitioner Relations – What role do you play in working with others? What are your expectations? Theirs? Before you sign on the dotted line, consider the implications of the business agreement you’re entering into. Learn how to strengthen relationships with your work mates and support staff. If you’re a business owner, effectively scale up to incorporate practitioners into your enterprise.
9) Perspective – Comprehend the extrinsic factors that influence your practice viability – government policy and funding, insurance industry and gatekeeper health practitioner relations, public and media endorsement, competitors and profiteers. Explore the profession’s culture and essential stakeholders as they exercise influence on your practice.
10) Promises and processes – Set practice policies and processes that deliver on your quality of care. Consider regulations and laws that govern your practice.
Actualized: Professional and Personal Maturation
11) Potential – Evaluate and entertain delivery-of-care models, discuss how to use tools, team and technology to reduce strain while increasing work capacity and income potential. Consider how to generate other sources of income.
12) Public & Private Good – Consider your contribution to public health and wellness initiatives, while nurturing the private good in your own well-being.
Write me with your suggestions at don@dondillon-RMT.com. Let’s elevate the profession together.
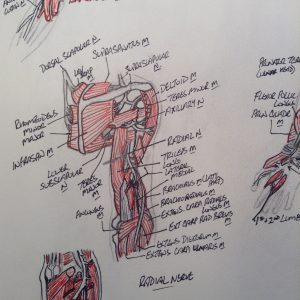
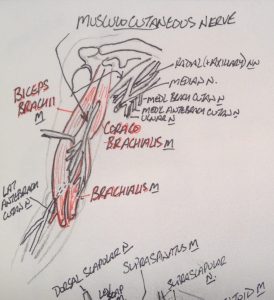
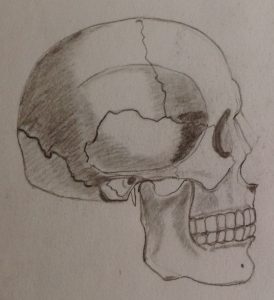
 How do you learn and appreciate anatomy? Did you use the Anatomy Colouring Book, or doodle, or find some other way to get it to stick in your memory? Can we use illustration to provide better representation of what we feel under our fingers, to give the public an in vivo look into the engagement of hands-to-body?
How do you learn and appreciate anatomy? Did you use the Anatomy Colouring Book, or doodle, or find some other way to get it to stick in your memory? Can we use illustration to provide better representation of what we feel under our fingers, to give the public an in vivo look into the engagement of hands-to-body? Calling all amateur anatomical illustrationalists out there…share your artwork!
Calling all amateur anatomical illustrationalists out there…share your artwork!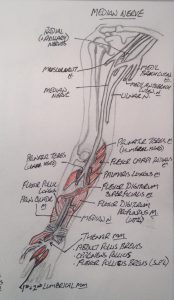




 Are you using your case history as a tool to reduce risk of harm? Would you like to build more competence in this skill? Have a look at the
Are you using your case history as a tool to reduce risk of harm? Would you like to build more competence in this skill? Have a look at the  Are you overwhelmed with the operations-side of running a practice? Have you inherited a mixed bag of useful practice tips coupled with antiquated and even incorrect guidance?
Are you overwhelmed with the operations-side of running a practice? Have you inherited a mixed bag of useful practice tips coupled with antiquated and even incorrect guidance?




